Eye Disease - Schedule an Appointment.
We are currently accepting new patients! Be sure to review the coverage of your insurance provider. We make it fast and convenient for you to schedule an appointment online at your convenience.Cataracts
While a comprehensive eye examination can determine for certain if you have a cataract forming, there are a number of signs and symptoms that may indicate a cataract.
Among them are:
- Gradual blurring or hazy vision where colors may seem yellowed
- The appearance of dark spots or shadows that seem to move when the eye moves
- A tendency to become more nearsighted because of increasing density of the lens
- Double vision in one eye only
- A gradual loss of color vision
- A stage where it is easier to see without glasses
- The feeling of having a film over the eyes
- An increased sensitivity to glare, especially at night
 What is a Cataract?
What is a Cataract?
A cataract is a clouding of the normally clear crystalline lens of the eye. This prevents the lens from properly focusing light on the retina at the back of the eye, resulting in a loss of vision. A cataract is not a film that grows over the surface of the eye, as is often commonly thought.
Why are They Called Cataracts?
Sometimes cataracts can be seen as a milkiness on the normally black pupil. In ancient times, it was believed this cloudiness was caused by a waterfall - or cataract - behind the eye.
Who Gets Cataracts?
Cataracts are most often found in persons over the age of 55, but they are also occasionally found in younger people, including newborns.
What Causes Cataracts?
It is known that a chemical change within the eye causes the lens to become cloudy. The change may be due to advancing age or it may be the result of heredity, an injury or a disease.
Excessive exposure to ultraviolet or infrared radiation present in sunlight or from furnaces, cigarette smoking and/or the use of certain medications are also cataract risk factors. Cataracts usually develop in both eyes, often at different rates.
Can Cataracts be Prevented and Treated?
Currently, there is no proven method to prevent cataracts from forming.
If your cataract develops to a point that daily activities are affected, you will be referred to an eye surgeon who may recommend the surgical removal of the cataract.
Prescription changes in your eyewear will help you see more clearly until surgery is necessary, but surgery is the only proven means of effectively treating cataracts. The surgery is relatively uncomplicated and has a very high success rate.
When Will I Need to Have Cataracts Removed?
Cataracts may develop slowly over many years or they may form rapidly in a matter of months. Some cataracts never progress to the point that they need to be removed. Usually, you will be ready to have the cataract removed when it is having a significant adverse effect on your lifestyle.
Our office will arrange a consultation with a surgeon who will decide on the appropriate time for removal. Most people wait until the cataracts interfere with daily activities before having them removed.
What Happens after Cataract Surgery?
You, along with your doctors, will decide on the type of post-cataract vision correction that you will use. Intraocular lens implants, inserted in your eye at the time of surgery, serve as a "new lens" and are the most frequent form of visual correction. In some cases, however, eyeglasses or contact lenses may also be needed to provide the most effective post-cataract vision.
Cataract surgery has now developed to the point where most procedures are completed in a day and overnight stays in hospital are unnecessary. The results are usually excellent and patients are often able to appreciate a significant improvement in vision almost immediately following surgery.
Diabetes
Diabetes, a disease that prevents your body from making or using insulin to break down sugar in your bloodstream, can affect your eyes and your vision.
Fluctuating or blurring of vision, intermittent double vision, loss of peripheral vision and flashes and floaters within the eyes may be symptoms related to diabetes. Sometimes the early signs of diabetes are detected during a thorough eye examination.
Diabetes can cause changes in nearsightedness and farsightedness and lead to premature presbyopia (the inability to focus on close objects). It can result in cataracts, glaucoma, a lack of eye muscle coordination (strabismus) and decreased corneal sensitivity. The most serious eye problem associated with diabetes is diabetic retinopathy, which, if not controlled, can lead to blindness.
What is Retinopathy?
Diabetic retinopathy occurs when there is a weakening or swelling of the tiny blood vessels in the retina of your eye, resulting in blood leakage, the growth of new blood vessels and other changes.
Can Vision Loss from DIabetes be Prevented?
Yes, in a routine eye examination, your eye care practitioner can diagnose potential vision-threatening changes in your eyes that may be treated to prevent blindness. However, once damage has occurred, the effects are usually permanent. It is important to control your diabetes as much as possible to minimize the risk of developing retinopathy.
How is Diabetic Retinopathy Treated?
In the early stages, diabetic retinopathy can be treated with laser therapy. A bright beam of light is focused on the retina, causing a burn that seals off leaking blood vessels. In other cases, surgery inside the eye may be necessary. Early detection of diabetic retinopathy is crucial. It is routinely screened for in an eye examination.
Are There Risk Factors for Developing Retinopathy?
Several factors that increase the risk of developing retinopathy include smoking, high blood pressure, excessive alcohol intake and pregnancy.
How can Diabetes-Related Eye Problems be Prevented?
Diabetes-related eye problems can be prevented by monitoring and maintaining control of your diabetes. See your physician regularly and follow instructions about diet, exercise and medication. A thorough eye examination when first diagnosed as a diabetic, at least annually thereafter, is recommended.
Dry Eye
If your eyes sting, itch or burn, you may be experiencing the common signs of "dry eye." A feeling of something foreign within the eye or general discomfort may also signal dry eye.
What is Dry Eye?
Dry eye describes eyes that do not produce enough tears. The natural tears that your eyes produce are composed of three layers:
- The outer oily layer, which prevents or slows evaporation of the tear film
- The middle watery layer; which moisturizes and nourishes the front surface of the eye
- The inner mucus layer, which helps maintain a stable tear film
Dry eye may occur because the volume of tears produced is inadequate (we all produce fewer tears as we get older, and in some cases this can lead to dry eye symptoms). It may result because the composition of the tears has changed so that they are unstable and evaporate more quickly.
What Causes Dry Eye?
Dry eye symptoms can result from the normal aging process. Exposure to environmental conditions, as well as medications, such as antihistamines, oral contraceptives or anti-depressants, can contribute to the symptoms of dry eye. Or, dry eye can result from chemical or thermal burns to the eye. Dry eye may also be symptomatic of general health problems or other diseases. For example, people with arthritis are more prone to dry eye.
Will Dry Eye Harm My Eyes?
If untreated, it can. Excessive dry eye can damage tissue and possibly scar the cornea at the front of your eye, impairing vision. Dry eye can make contact lens wear more difficult since tears may be inadequate to keep the lenses wet and lubricated. This can lead to irritation and a greater chance of eye infection. Therefore, it is important to follow the recommended treatment plan.
How is it Diagnosed?
During the examination, you will be asked about your general health, use of medications, and work and home environments to determine factors, which may be contributing to dry eye symptoms. This information will help decide whether to perform specific dry eye tests.
To test for dry eye, diagnostic instruments that allow a highly magnified view of your eyes or small strips of paper or thread and special dyes to assess the quantity and quality of the tears may also be used.
How is it Treated?
Dry eye cannot be cured, but your eyes' sensitivity can be lessened and measures taken so your eyes remain healthy. The most frequent method of treatment is the use of artificial tears or tear substitutes.
For more severe dry eye, ointment can be used, especially at bedtime. In some cases, small plugs may be inserted in the corner of the eyelids to slow drainage and loss of tears.
To keep dry eye symptoms in check, you and your optometrist need to work together. If you have increased dryness or redness that is not relieved by the prescribed treatment, let us know as soon as possible.
glaucoma
The build-up of pressure inside your eye leads to glaucoma. Aqueous fluid, which fills the space at the front of the eye just behind the cornea, is made behind the iris (the colored part of the eye) in the ciliary body. It flows through the pupil (the dark hole in the center of the iris), and drains from the 'anterior chamber angle,' which is the junction between the edge of the iris and the cornea. If this outflow of liquid is impaired at all, there is a build-up of pressure inside the eye that damages the optic nerve, which carries visual images to the brain. The result is a loss of peripheral vision. Thus, while glaucoma sufferers may be able to read the smallest line on the vision test, they may find it difficult to move around without bumping into things or to see moving objects to the side.
Tests for glaucoma are part of a comprehensive eye examination. A simple and painless procedure called tonometry measures the internal pressure of your eye. Ophthalmoscopy examines the back of the eye to observe the health of the optic nerve. A visual field test, a very sensitive test that checks for the development of abnormal blind spots, may also be completed.

What Causes Glaucoma?
Some causes are known, others are not. Causes differ depending on the type of glaucoma. The exact cause of open-angle glaucoma, where the drainage channels for the aqueous appear to be open and clear, is not known. Closed-angle glaucoma can occur when the pupil dilates or gets bigger and bunches the iris up around its edge, blocking the drainage channel. An injury, infection or tumor in or around the eye can also cause internal eye pressure to rise either by blocking drainage or displacing tissues and liquid within the eye. A mature cataract also can push the iris forward to block the drainage 'angle' between the iris and the cornea. Glaucoma can occur secondarily to a number of other conditions, such as diabetes, or as a result of some medications for other conditions.
Who gets Glaucoma?
Glaucoma most frequently occurs after age 40, but can occur at any age.
If you're of African heritage, you are more likely to develop open-angle glaucoma -- and at an earlier age -- than if you're Caucasian. Asians are more likely to develop narrow-angle glaucoma.
You have a higher risk of developing glaucoma if a close family member has it or if you have high blood pressure or high blood sugar (diabetes). There is also a greater tendency for glaucoma to develop in individuals who are nearsighted. Those at heightened risk for glaucoma should have their eyes checked at least once a year.
Why is Glaucoma Harmful to Vision?
The optic nerve, located at the back of the eye, carries visual information to the brain. As the fibers that make up the optic nerve are damaged by glaucoma, the amount and quality of information sent to the brain decreases and a loss of vision occurs.
Will I Go Blind from Glaucoma?
If diagnosed at an early stage, glaucoma can be controlled and little or no further vision loss should occur. If left untreated, side awareness (peripheral vision) and central vision will be destroyed and blindness may occur.
How is Glaucoma Detected?
The most scary thing about glaucoma is that it can steal your vision gradually and without your noticing. The best defense against glaucoma is a regular eye examination. Glaucoma most often strikes people over age 50. But it is recommended that during adult life everyone be tested at least every two years.
Some people with glaucoma do experience symptoms, but symptoms vary depending on the type of glaucoma.
Primary Open-Angle Glaucoma
By far the most common type, primary open-angle glaucoma develops gradually and painlessly. Since there are no early warning signs, it can slowly destroy your vision without your knowing it. The first indication may only occur after some considerable vision loss.
Acute Angle-Closure Glaucoma
This results from a sudden blockage of the drainage channels within your eye, causes a rapid build-up of pressure inside your eye accompanied by blurred vision, the appearance of colored rings around lights and sometimes extreme pain or redness in the eyes.
How is Glaucoma Treated?
Glaucoma is usually treated with prescription eye drops and medicines. In some cases, surgery may be required to improve drainage. The goal of the treatment is to prevent loss of vision by lowering the pressure in the eye.
Will My Vision be Restored After Treatment?
Unfortunately, any vision loss as a result of glaucoma is permanent and cannot be restored. This is why regular eye examinations are important.
Glaucoma cannot be prevented, but early detection and treatment can control glaucoma and reduce the chances of damage to the eye and a loss of sight.
Conjunctivitis (PInk Eye)
Red, watery eyes, inflamed lids, blurred vision and a sandy or scratchy feeling in the eyes may indicate that you have conjunctivitis. Pus-like or watery discharge around the eyelids may indicate an infectious form of the disease, commonly known as "pink eye."
Conjunctivitis is an inflammation or infection of the conjunctiva, a thin, transparent layer covering the surface of the inner eyelid and the front of the eye. It affects people of all ages.
What Causes Conjunctivitis?
The three main types of conjunctivitis are infectious, allergic and chemical. The infectious form, commonly known as "pink eye," is caused by a contagious virus or bacteria. Your body's allergies to pollen, cosmetics, animals or fabrics often bring on allergic conjunctivitis. Irritants like air pollution, noxious fumes and chlorine in swimming pools may produce the chemical form.
It is Important to Prevent Spreading Conjunctivitis.
If contagious, measures can be taken to prevent spreading conjunctivitis to others.
- Keep your hands away from your eyes
- Thoroughly wash hands before and after applying eye medications
- Do not share towels, washcloths, cosmetics, or eyedrops with others
- Seek treatment promptly
Small children, who may forget these precautions, should be kept away from school, camp, and the swimming pool until the condition is cured.
Certain forms of conjunctivitis can develop into a serious condition that may harm your vision. Therefore, it is important to have conjunctivitis diagnosed and treated quickly.
How is Infectious Conjunctivitis Treated?
Infectious conjunctivitis, caused by bacteria, is usually treated with antibiotic eye drops and/or ointment. Other infectious forms, caused by viruses, can't be treated with antibiotics and must be fought off by your body's immune system. On occasions antibiotics may be prescribed to prevent secondary bacterial infections from developing.
How are the Allergic and Chemical Forms of Conjunctivitis Treated?
The ideal treatment for both forms is to remove the cause of the allergy or irritation. For instance, avoid contact with any animal if it causes an allergic reaction. Wear swimming goggles if chlorinated water irritates your eyes. In cases where these measures won't work, prescription and over-the-counter eye drops are available to help relieve the discomfort.
Macular Degeneration
Macular degeneration (AMD) is the leading cause of blindness in patients 55 years of age and older. I would like to share some of the latest studies and science surrounding this mostly preventable blinding eye disease. Current research shows that some carotenoids and omega-3 fatty acids(fish oil) could have a major impact on delaying the onset of blindness resulting from AMD. Carotenoids are organic pigments found in natural foods such as fruits and vegetables, which contain beneficial antioxidants. Sufficient intake of the carotenoids, 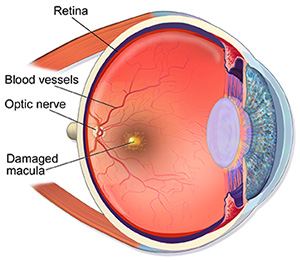 zeaxanthin and lutein, may reduce the risk of blinding effects from AMD by as much as 93%. Lutein is found in dark leafy green vegetables such as spinach, collard greens, and Kale. Finding a large amount of zeaxanthin in food is more difficult, but smaller amounts can be obtained from orange bell peppers, egg yolks, oranges and Goji berries. Dr. Stuart Richer of the Veterans Administration and others have shown through research that increasing lutein and zeaxanthin levels in the macula can improve your visual acuity, color vision, light sensitivity, contrast and small amounts of visual distortion. Many researchers believe that zeaxanthin is actually more important than lutein because it resides in the center of the macula, whereas lutein is found in greater porportion in the macular periphery.
zeaxanthin and lutein, may reduce the risk of blinding effects from AMD by as much as 93%. Lutein is found in dark leafy green vegetables such as spinach, collard greens, and Kale. Finding a large amount of zeaxanthin in food is more difficult, but smaller amounts can be obtained from orange bell peppers, egg yolks, oranges and Goji berries. Dr. Stuart Richer of the Veterans Administration and others have shown through research that increasing lutein and zeaxanthin levels in the macula can improve your visual acuity, color vision, light sensitivity, contrast and small amounts of visual distortion. Many researchers believe that zeaxanthin is actually more important than lutein because it resides in the center of the macula, whereas lutein is found in greater porportion in the macular periphery.
People at greatest risk for developing AMD are those with a family history of the disease, those who eat high glycemic foods or foods high in trans fats, smokers, people age 55 and older, couch potatoes and people who have low amounts of lutein and zeaxanthin in the macula (macular protective pigment). Doctors can now test how much pigment (lutein and zeaxanthin) is in the macula, i.e.- low density of macular protective pigment signifies greater risk for developing macular degeneration. Unfortunately, the average American diet does not consist of the necessary amounts of zeaxanthin and lutein. Eating a regular diet consistiong of leafy green vegetables and deep water oily fish (ex.- salmon, mackerel, halibut, sardines, anchovies) may successfully increase macular protective pigment density by up to 80% within 6 months. For those that may have trouble adhearing to this form of diet, your doctor can prescribe eye supplements that contain these important nutrients to reduce your risk or delay the onset of developing this horrific blinding eye disease. Preventive eyecare, including patient education and intervention, is the newest frontier in the quest for maintaining healthy eyes and preventing vision loss.
Easily Order Your Contacts Online
Our eye care patients are able to now easily reorder their contacts online through our secure store. We simply approve your prescription and process your order. Break up annual supply costs with EyeSubscribe!
Contact Our Optometry Group
In order to permit us to best respect your time, we encourage appointments. However, we also recognize your busy schedule may not always permit this, and we make every effort to accommodate patients on a walk-in basis.
Office Hours: Monday - Friday: 10:00 am - 6:00 pm • Saturday: 10:00 am - 4:00 pm • Sunday: 11:00 pm - 5:00 pm
Address
Located in SouthPark Mall4400 Sharon Road, Charlotte, NC